Medication management across the health system can be complex. Drugs requiring refrigeration make workflow management and proper storage even more complicated. For this reason, USP Chapter <1079> provides guidance around maintaining the cold chain. Many health systems and pharmacies are looking to upgrade cold storage units due to increased pressure from storage guidelines and recommendations as well as the high risks related to the improper storage of refrigerated drugs. USP <1079> outlines seven key recommendations to ensure your pharmaceutical storage units are always storing drugs safely within the manufacturer’s recommended temperature range. Each recommendation will be covered in detail throughout this paper.
Risks of Improper Storage
Preparations which take several routes before reaching the patient are at higher risk of temperature excursions, exposure to humidity, light and oxygen. Individuals must have systems in place to track and record storage conditions throughout the cold chain to ensure drug efficacy, patient safety, and protection from financial loss due to wasted refrigerated medications.
There is great risk associated with medication being compromised by exposure to temperatures beyond the safe temperature range determined by the manufacturer. “The loss of efficacy can result in many issues compromising the health of the patient. With some medications, the stakes are even higher. If epinephrine, for example, is exposed to repetitive heating and cooling, it can lose 64% of its efficacy. If a compromised dose of epinephrine is used to treat a patient suffering from a serious anaphylactic reaction, it may not work as intended, resulting in possible death (Katzki).”
Financial Burden
Another risk of storing medications out of the manufacturer’s recommended temperature range is financial loss. Drugs stored at out of range temperature for significant periods of time may become ineffective and must be disposed of. Some refrigerated drugs may be short dated and stored at ambient temperature significantly reducing the life of the drug. This increases the risk of the drug expiring before use leading to waste and amplified financial burden.
GENERAL CHAPTER <1079>
General Chapter <1079> provides guidance concerning storage, distribution, and shipping of pharmacopeial preparations. This article focuses on the area of the chapter which describes essential procedures to maintain proper storage environments for temperature sensitive drugs to ensure a preparation’s integrity from prep to administration. There is a vast set of testing data recommended to ensure temperature-controlled storage environments maintain appropriate conditions for temperature sensitive drugs. Understanding and measuring temperature uniformity, stability, and recovery ensures drugs are stored according to manufacturer instructions.
USP <1079> reinforces that good practices are necessary for all temperature-controlled pharmaceuticals. The chapter explains the temperature ranges for drugs stored at the following requirements:
- Room Temperature Storage: 20°C – 25°C (Excursions permitted between 15°C and 30°C)
- Controlled Room Temperature: 20°C – 25°C
- Cool Storage: 8°C – 15°C
- Refrigerator Storage: 2°C – 8°C
- Freezer Storage: -25°C – 10°C
Other storage parameters such as, “store in a cool dry place or protect from light,” provide guidance on how to properly store various drugs which may be sensitive to humidity or light.
FOLLOWING USP <1079> STORAGE RECOMMENDATIONS
The chapter outlines seven key recommendations to ensure drugs are stored safely and within the correct temperature ranges. The use of medical-grade refrigerators, stability testing, uniformity testing, recovery testing, temperature monitoring, personnel training, and regular calibration will ensure drugs are stored within the recommended temperature ranges to prevent excess waste, patient harm, and financial burden. Each USP <1079> Good Drug Storage Practice is outlined below in further detail.
#1 Medical-Grade Cold Storage Equipment
Most pharmaceuticals will have storage conditions noted on their labeling. Preparations which require storage at “cool,” “cold,” “refrigerator,” or “freezer temperatures will need to be stored in units designated to maintain these conditions. Equipment should be qualified according to written procedures provided by the management system.
The use of medical-grade refrigerators is highly recommended for drug storage. CDC recommends purpose-built or pharmaceutical-grade units designed to either refrigerate or freeze. The Joint Commission also references these CDC recommendations when referring to refrigerated drug storage. These units can be compact, under-the-counter style or large. Purpose-built units, sometimes referred to as “pharmaceutical grade,” are designed specifically for storage of biologics, including vaccines (CDC).
These units often have:
- Microprocessor-based temperature control with a digital temperature sensor (thermocouple, resistance temperature detector [RTD], or thermistor)
- Fan-forced air circulation with powerful fans or multiple cool air vents promoting uniform temperature and fast temperature recovery from an out-of-range temperature.
- Pharmaceutical-grade refrigeration provides stable, uniform temperatures to safeguard temperature sensitive medications requiring refrigeration. Medical-grade refrigeration manufacturers should be able to provide you the data recommended to have on file by the USP <1079> General Chapter - Good Drug Storage and Shipping Practices.
#2 Stability Testing
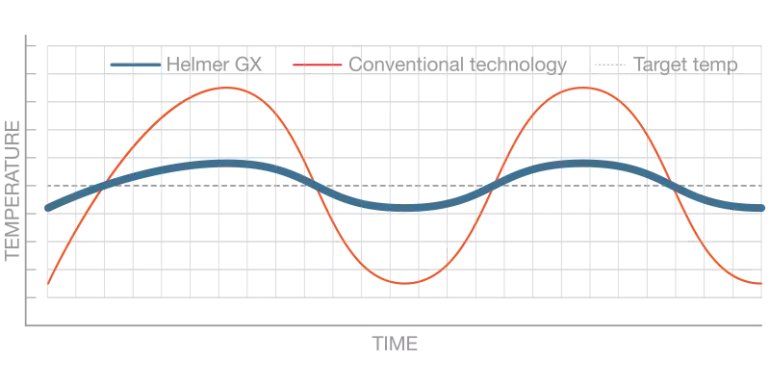
Temperature stability measures how effectively the cold storage unit maintains temperature at setpoint, even during compressor and auto-defrost cycles.
Only climate-controlled equipment for which a contractor has provided documentation to assure suitability for temperature and humidity requirements should be considered. Qualification procedures should be independently conducted on a regular basis to guarantee stability and proper functionality. The procedure should document the temperature profile for both air and product temperatures when the equipment is empty and when it is loaded. In addition, it should be documented how long it takes for temperatures to exceed the maximum limit in the event of a power failure, as well as how door opening and stocking effects storage temperature.
Figure 1. Temperature Stability
#3 Uniformity Testing
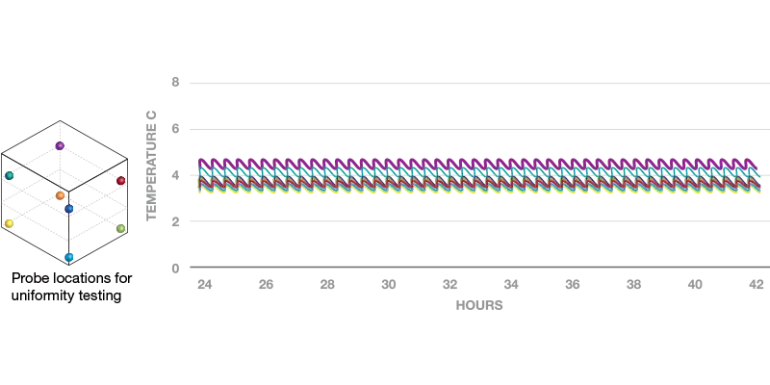
Temperature uniformity is the measurement of temperature consistency across all usable locations in the cabinet. Tight uniformity provides confidence that contents are maintained at the correct temperature regardless of storage location. Non-medical-grade equipment may have poor uniformity performance and can include hot and cold spots that cause product to go out of temperature range. This can create both safety and regulatory risks. Therefore, many clinical applications, such as medication storage, require the use of higher quality cold storage.
Testing should prove that the equipment can maintain required temperature ranges in all locations of the unit. Any areas which should not be used for storage (cooling coils, cold air streams, doors etc.) must be defined. Temperature monitoring should establish that the system is able to maintain proper temperatures consistently and reliably.
Figure 2. Temperature Uniformity
#4 Recovery Testing
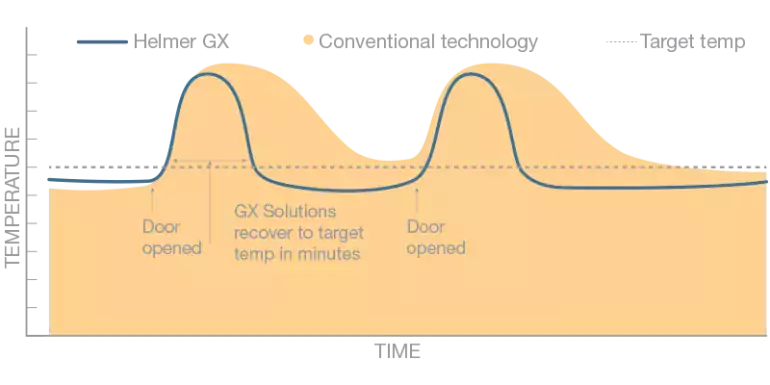
Temperature recovery is the measurement of the time required for a cold storage cabinet to return to after the temperature set point after a door opening. Quick temperature recovery is necessary to ensure that door openings do not cause products to go out of tight temperature ranges required for clinical products.
A study conducted by NIST in 2016 determined that in a clinic setting, refrigerators may be accessed by staff over 30 times in a single hour. Temperature recovery performance is also critical when considering extended door openings due to inventory counts or restocking.
Figure 3. Temperature Recovery
#5 Temperature Monitoring
Temperature monitoring equipment can be used to measure air or product temperatures at regular intervals. USP <1079> states that temperatures should be examined at least once every 24 hours or more depending on what your protocol outlines. Some monitoring equipment has the capability to alarm or alert staff if temperature goes out of range.
The CDC provides additional, detailed information on temperature monitoring devices for vaccine storage units, and this information applies the same way for refrigerators storing other temperature sensitive medications.
CDC recommends a specific type of TMD called a “digital data logger” (DDL). A DDL provides the most accurate storage unit temperature information, including details on how long a unit has been operating outside the recommended temperature range (referred to as a “temperature excursion”). Unlike a simple minimum/maximum thermometer, which only shows the coldest and warmest temperatures reached in a unit, a DDL provides detailed information on all temperatures recorded at preset intervals.
Many DDLs use a buffered temperature probe, which is the most accurate way to measure actual vaccine temperatures. Temperatures measured by a buffered probe more closely match vaccine temperatures than those measured by standard thermometers, which tend to reflect only air temperature.
Temperature data from a DDL can either be downloaded to a computer using special software or retrieved from a website. The software or website may also allow you to set the frequency of temperature readings. Reviewing DDL data is critical for pharmaceutical viability, so it is important to decide whether independent software or a website program works best for your facility (CDC).
#6 Personnel Training
It is important to not only use temperature monitoring, but to have controls in place to address the steps necessary for responding to temperature excursions both inside and outside of working hours. All personnel who handle medications which require refrigeration should be provided with proper training on how to monitor temperatures and react to temperature excursions.
Ensure there are standards in place to train personnel on how to handle, document, and record any adverse events. Records should explain the reason for the temperature deviation and the resulting action taken (including if the preparation will be issued to the patient). The pharmacy should seek advice on the stability and whether it is safe for administration from the product manufacture or supplier.
#7 Calibration & Maintenance
All equipment used for recording, monitoring, and maintaining temperatures should be calibrated to NIST, ISO17025 or international standards on a regular basis. The calibration of all monitoring devices (including alarms) should be checked on an annual or semiannual basis. Regular maintenance protocols should be in place and documented for all refrigeration equipment. Many pharmaceutical grade manufacturers can offer certificates of calibration with new equipment purchases.
CONCLUSION
There is risk of loss of efficacy, patient harm, and financial loss when drugs requiring refrigeration are stored at out of range temperatures. USP General Chapter <1079> outlines good storage practice for temperature sensitive drugs during all phases of the cold chain. Using the right cold storage equipment can play a significant role in reducing risk related to refrigerated drugs. Temperature monitoring and personnel training may also help streamline the storage of refrigerated drugs. Proper refrigerated storage is an important part of medication management.
REFERENCES
- USP. USP 39–NF 34. <1079> Good Storage and Distribution Practices for Drug Products, Rockville, MD: United States Pharmacopeial Convention; 2016
- Katzki, Dan. “Temperature-Sensitive Medications.” Specialty Pharmacy Times, 17 Dec. 2013, https://www.specialtypharmacytimes.com/publications/specialty-pharmacy-times/2013/nov_dec-2013/temperature-sensitive-medications/p-2.